Interview with Prof. Patrick Santens, neurologist at University Hospital Ghent and Professor of Neurology at Ghent University
“Parkinson’s disease is currently the fastest growing neurodegenerative disease, also in young people. It’s true to say that there is a real pandemic.” says Professor Patrick Santens, neurologist at University Hospital Ghent and Professor of Neurology at Ghent University. Unfortunately, the figures in Belgium and worldwide appear to support this observation. In view of World Parkinson Day 11 April 2022, we interviewed Patrick Santens about his insights into this disease.
Confrontational figures
Patrick Santens confirms the figures on Parkinson’s
disease that we recorded back in April 2021 during an interview with Karl Wouters, founder of medinet.tv and board member of the Flemish Parkinson Association: “Based on extrapolations from worldwide population surveys, we can state that Belgium has around 35,000 Parkinson’s disease patients. In Europe there are more than 1.2 million
patients, and worldwide no fewer than 10 million.
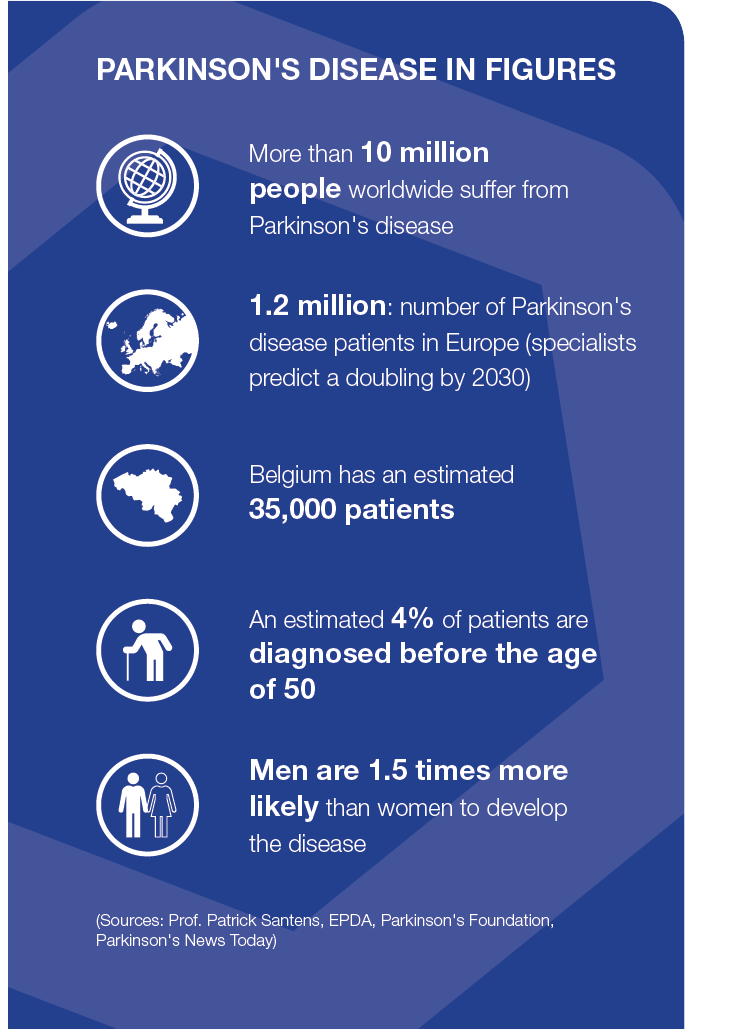
The rapid increase in the number of patients under the age of 50 is particularly worrying. These rising figures, which are a global phenomenon, can be explained in part by the increasing ageing population and higher life expectancy, including in developing countries, than seen in previous times. It’s therefore safe to speak of a real Parkinsonian pandemic, referring to the term used by my Dutch colleague Prof. Bas Bloem in his book ‘De Parkinson Pandemie. Een recept voor actie’.”
New insights into Parkinson’s disease
What is Parkinson’s disease? According to Patrick Santens, the answer to this seemingly simple question has become much more complex than it was a few years ago. “In the past, the answer would have been as follows:
a neurodegenerative disorder of the central nervous system, in which dopamine-producing cells die, resulting in characteristic changes in the motor skills of patients.
Today, as a result of new insights into the disease, we know that this is only part of the story. After all, there is more to Parkinson’s disease than the disappearance of dopamine-generating cells. In addition to an impairment
of the central nervous system, other organs in the body can also be affected. This leads to additional non-motor symptoms.”
“So, there doesn’t seem to be just one kind of Parkinson’s disease. From a clinical point of view, no two patients with Parkinson’s disease are the same. It is apparent that the disease remains dormant for a long time before motor symptoms manifest in a person. We know this from more recent research, which shows a pathological impairment – that has sometimes been going on for years – of a number of systems inside and outside the brain.”
“Another important finding is that the disease does not occur in the same way in all patients. There are purely genetic forms of the disease (less than 10%), but in the vast majority of patients there are no direct indications of hereditary components. We, therefore, look at environmental factors and at the interaction between hereditary and environmental factors. This often results in a different progression. However, we still know too little about this.”
“We can conclude that there are different forms of the disease, but with overlapping characteristics and a high degree of heterogeneity within the spectrum of the disease.”
All bugs: the role of microbiomes
Interesting new knowledge has also been gathered in recent years about the development of Parkinson’s disease. Among other things, Patrick Santens refers to new information on the role of the microbiome – the collective name for microorganisms that colonise the human body – as a possible trigger. “The different organs in our bodies each have their own microbiome. Take, for example, the totality of microorganisms in the respiratory tract or the intestinal system. Both channels are entry points through which substances enter the body from the outside. About 10 years ago, scientists specialising in intestinal biopsies discovered protein deposits (so-called ‘alpha-synuclein deposits’) in the neurons of the intestinal wall. The individuals in whom such protein deposits were found later developed Parkinson’s disease. These findings triggered new questions. Does the disease develop outside of the nervous system? And if so, then why in the intestinal system? New studies have already shown that the microbial composition of intestinal contents is different in patients with Parkinson’s disease than in those without the disease, for example with a more pro-inflammatory intestinal content. People suffering from ulcerative colitis or Crohn’s disease would also be more prone to Parkinson’s disease.”
“The respiratory and oral microbiome also seem to play a role in the development of the disease. For example, we know that loss of smell is one of the first premotor symptoms of Parkinson’s disease. The damage to the olfactory nerve can be related to polluted air that someone inhales every day, with particles that cause inflammation. Today, we also know that the oral microbiome in Alzheimer’s patients differs significantly compared with non-Alzheimer’s patients. These are avenues that we must continue to explore…”
Environmental factors: from smoking to pesticides
In addition to the possible impact of the microbiome on the development of Parkinson’s disease, Patrick Santens also points to environmental factors. “Today, there is sufficient epidemiological evidence to suggest that various environmental factors help facilitate the development of the disease. Surprisingly, smokers are less likely to develop the disease. The same goes for people who drink a lot of coffee. Even drinking milk can have a potential impact. This is where the presence of pesticides in our food comes into play. Because certain residues of pesticides may be present in milk products. Did you know that in France, Parkinson’s disease is recognised as an occupational disease for farmers who often work with pesticides?”
“However, a lot of research is still needed in the area of environmental factors. What possible role do diesel particles, particulate matter or even radiation from mobile phone masts play in the possible development of the disease? In the short term, these external factors do not appear to be a threat, but what about the longer term? In cardiovascular diseases or certain cancers, medical science today can point to specific ‘killers’. But, in neurodegenerative pathologies, the effect of long-term exposure plays a role, with a combination of the factors of time and interaction. For example, are smokers protected against Parkinson’s disease because there are protective substances in cigarette smoke, or do smokers – because of the fact that they regularly light a cigarette – have a different dopamine system than non-smokers?’
Treatment options, challenges,
and current research
Treatment options for Parkinson’s disease comprise dopamine-replenishing, symptomatic therapies; however, there remains a substantial unmet medical need because no treatments are currently available that actually stop or reverse disease progression.1
Among the greatest challenges in drug development for Parkinson’s disease are the number of biological pathways and proteins involved in the underlying disease pathogenesis, as well as the complexity of the affected organs (mainly the brain), and the aggressiveness of the disease itself.2 Accordingly, the need to develop novel drugs for Parkinson’s disease is prompting the pharmaceutical industry to utilise new methodologies when designing and developing new compounds.
Current trends in Parkinson’s disease research are shifting more towards personalized treatments that target the restoration of molecular, anatomical, and functional integrity of disease-specific brain circuits.1
What new treatments are being developed?3
Investigational new treatments are being evaluated in clinical studies, which have the potential to slow, halt, or reverse Parkinson’s disease. These include:
- Stem cell therapies, based on using healthy, living cells to replace or repair the damage to brain matter caused by Parkinson’s disease
- Gene therapies, based on using genetics to reprogramme cells and change their behaviour to help them remain healthy and continue to function for longer
- Growth factors (such as glial cell line-derived neurotrophic factor [GDNF]), based on using naturally occurring molecules that support the growth, development, and survival of brain cells
Sources:
1 Ntetsika T, et al. Mol Med. 2021;27:17; 2 Cruz-Vicente, Molecules 2021; 3 Parkinson’s UK website. Accessed 6 April 2022. https://www.parkinsons.org.uk/research/when-will-there-be-cure-parkinsons)
Treatment of Parkinson’s disease: ‘work in progress’
How does Patrick Santens see the treatment of Parkinson’s disease evolving? He explains: “Unfortunately, there is no treatment at present that heals or slows down the progression of the disease. On the one hand, we have a drug treatment that mainly fights the symptoms, and, on the other hand, a non-drug (i.e., paramedical) treatment that plays an important supportive role in the rehabilitation of patients.”
“Pharmaceutical companies are making many innovative efforts and developments in the field of drug treatment, although the focus remains primarily on modifying the dopamine system. The availability of new forms of administration and therapies – such as subcutaneous injection, transdermal administration or inhalation treatment approaches – provides additional comfort for patients, but has not (yet) led to a radically different approach in the fight against Parkinson’s disease. Today, there is a kind of stalemate as far as drug treatment is concerned, which means that patients are still unable to find solutions to sufficiently improve their quality of life. For advanced therapies, such as deep brain stimulation, the threshold is still quite high, partly because of the enormous cost (10,000 to 20,000 euros per implant).”
Importance of big data in research
Measuring is knowing. This principle also applies to research into the causes, symptoms, and treatment methods of Parkinson’s disease. In this context, Patrick Santens firmly believes in the role and usefulness of ‘big’ data. “We want to collect as much data as possible from certain target groups in the population in order to discover patterns of contamination. This can provide us with valuable information about potential interactions, possibly combined with genetic patterns. Within the University Hospital Ghent, we are currently working on a large-scale population survey to monitor several thousand Ghent residents over the course of a few years. The city of Ghent is supporting us here with the logistics. This research was developed from an idea I had to analyse how dietary patterns can affect (the development of) Parkinson’s disease. The rollout of this population survey can once again provide us with a great deal of interesting scientific knowledge.”
Bio
Professor Patrick Santens

Patrick Santens is a neurologist at the University Hospital Ghent (2004 – X) and Professor of Neurology at Ghent University (2013 – X).
His main specialisation is in the field of movement disorders, in particular Parkinson’s disease and related conditions. Since 2017, he has also had a 50% basic clinical mandate with the Research Foundation – Flanders (FWO).
Patrick Santens is a member of various working groups and scientific associations, including the Flemish Association for Neurology, the Belgian Association for Neurology and the Movement Disorder Society. He is co-author of more than 250 publications and annually publishes numerous articles in national and international journals.
Inspiring websites
- Vlaamse Parkinson Liga: www.parkinsonliga.be
- Parkinson’s UK: www.parkinsons.org.uk
- European Parkinson’s Disease Association: www.epda.eu.com
- The Michael J. Fox Foundation for Parkinson’s Research:
www.michaeljfox.org - Medinet TV:
www.medinet.tv
