Hereditary Angioedema – A Rare and Debilitating Disorder
Today is Rare Disease Day, so we wanted to take this opportunity to raise awareness of hereditary angioedema (HAE) – a rare disease that we have a lot of expertise in, here at BEYOND Communication.
Although affecting a relatively small proportion of the population, HAE can significantly disrupt the lives of patients and their families (see Fig. 1).1, 2 HAE is a genetic disorder, primarily mediated by bradykinin and changes in vascular permeability, characterized by recurrent episodes of subcutaneous or submucosal swelling (edema) affecting various parts of the body.1, 3-5 HAE symptoms can manifest at any age, but typically appear during childhood or adolescence, worsen during puberty, and persist throughout life.4, 6 Angioedema attacks are often painful, debilitating and potentially life-threatening.1, 2, 4 HAE has an unpredictable clinical course,1, 2 and many attacks occur without an obvious trigger.1, 4, 6 The estimated global prevalence of HAE is 1:50,000 people, but is likely to be higher due to delayed diagnosis and/or misdiagnosis.1-4, 6 Early detection and accurate diagnosis of HAE are crucial for appropriate treatment of the disorder and for preserving patients’ quality of life.4 A number of relevant published guidelines are available that provide specific clinical recommendations:
- World Allergy Organization/European Academy of Allergy and Clinical Immunology (WAO/EAACI)2
- International/Canadian Hereditary Angioedema Guideline7
- United States Hereditary Angioedema Association Medical Advisory Board (US HAEA MAB)8
HAE is a rapidly evolving therapeutic area and, thankfully, an increasing number of effective treatments (both for on-demand and prophylactic use) are emerging for patients with HAE – but that will be a topic for another day!
Figure 1: HAE is associated with a substantial and multifaceted burden of illness.
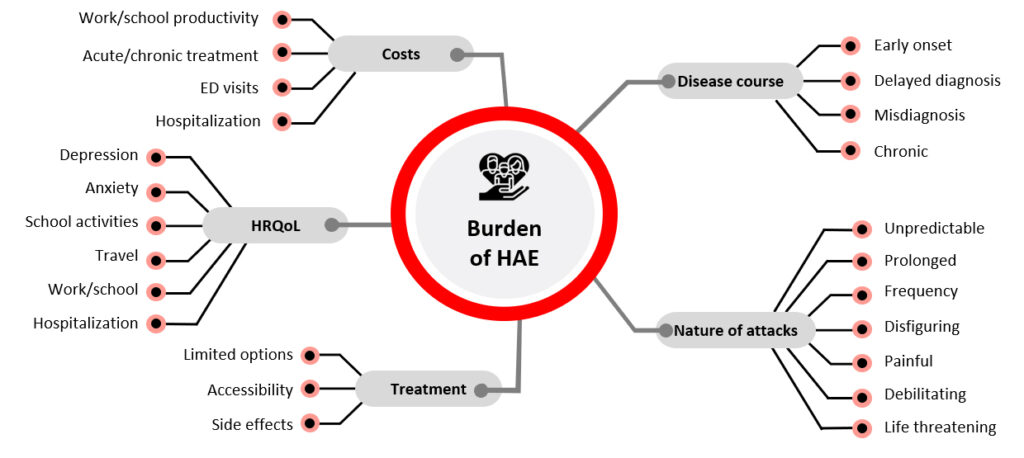
ED, emergency department; HAE, hereditary angioedema; HRQoL, health-related quality of life Adapted from Banerji A, et al. Ann Allergy Asthma Immunol. 2013;111:329–336.
References
1. Banerji A. Ann Allergy Asthma Immunol. 2013;111:329–336; 2. Maurer M, et al. Allergy. 2018;73:1575–1596; 3. Lumry WR. Am J Manag Care. 2013;19:s111–118; 4. Lumry WR. Am J Manag Care. 2013;19:s103–110; 5. Maas C, López-Lera A. Mol Immunol. 2019;112:378–386; 6. Farkas H, et al. Allergy. 2017;72:300–313; 7. Betschel S, et al. Allergy Asthma Clin Immunol. 2019;15:72; 8. Busse PJ, et al. J Allergy Clin Immunol Pract. 2021;9:132–150